GENERAL MEDICINE CASE DISCUSSION
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
THE CASE :
A 28 year old female resident of Nalgonda came to the medicine department with the chief complaints of nausea and vomiting since last 3 days.
History of presenting illness :
The patient was apparently asymptomatic 3 days ago. Then she had episodes of vomiting and loose stools.
Vomiting : sudden in onset , non billious , non projectile, with burning type of pain abdomen and with clear contents with the frequency of every 10 minutes.
Loose stools : sudden in onset , watery in consistency and not associated with mucus or blood with the frequency of every 10 minutes.
There is no history of :
Fever,
Dysphagia,
Abdominal distension,
Haematemesis,
Pedal edema.
Past History:
The patient similar episode 1 year back.
She is not a known case of Diabetes Mellitus , Hypertension, Bronchial asthma.
Family History:
No significant family history.
Personal history:
Diet : Mixed
Appetite : Normal
Bowel and bladder movements : Regular
Sleep - Adequate
No addictions
General Examination:
The patient conscious, coherent, cooperative and moderately built and is comfortably lying on the bed.
Pallor : Present
Icterus : Absent
Cyanosis : Absent
Koilonychia : Absent
Lymphadenopathy : Absent
Edema : Absent
VITALS :
Temperature : Afebrile
Pulse rate : 86 beats per minute
Respiratory rate : 18 cycles per minute
Blood Pressure : 110/70 mm of Hg.
Systemic Examination :
GASTROINTESTINAL SYSTEM :
A) Upper gastrointestinal tract :
Lips : Dry
Teeth : Normal
Gums : Normal
Tongue : Dry
Tonsils : Normal
Palate : Normal
Breath : No foul smell
B) Examination of the Abdomen :
I. Inspection : The legs of the patient are in extended position.
1. Shape of the Abdomen: Scaphoid
2. Flanks : not full
3. Venous prominence : Absent
4. Umbilicus : central in position, no discoloration
5. Skin : Absence of ulcer , striae , pigmentation,
Lower segment cesarean section scar present.
6. No localised swelling
7. Movement of the abdomen : quadrants moving with respiration, no pulsations or visible peristalsis.
II. Palpation:
1. Superficial :
a) Surface temperature : no local rise
b) Tenderness : Absent
c) Consistency : Normal elastic
d) Localised lump : Absent
e) Pulsations : Absent
f) Fluid thrill : Absent
2. Deep :
a) Liver : not palpable
b) Spleen : not palpable
c) Kidneys : not palpable
d) Rebound tenderness : Absent
e) Abdominal mass : Absent
III. Percussion :
1. General note of the abdomen : Present
2. No liver of splenic dullness
3. No shifting dullness
IV. Auscultation :
1) Bowel sounds heard
2) Hepatic or splenic rub : Absent
3) Bruit : Absent
RESPIRATORY SYSTEM:
1 . Position of trachea : Central
2. Normal vesicular breath sounds
3. No crepitation or Ronchi
CARDIOVASCULAR SYSTEM:
Normal S1 and S2 heard
No murmurs heard
CENTRAL NERVOUS SYSTEM:
1) Higher mental functions : Intact
2) Cranial nerves : Intact
3) Motor system : Normal
4) Sensory system : Normal
5) Reflexes : Intact
6) Cerebellar functions : Intact
Provisional Diagnosis :
Acute Gastroenteritis
Differential diagnosis :
Hepatitis
Peptic ulcer
Investigations:
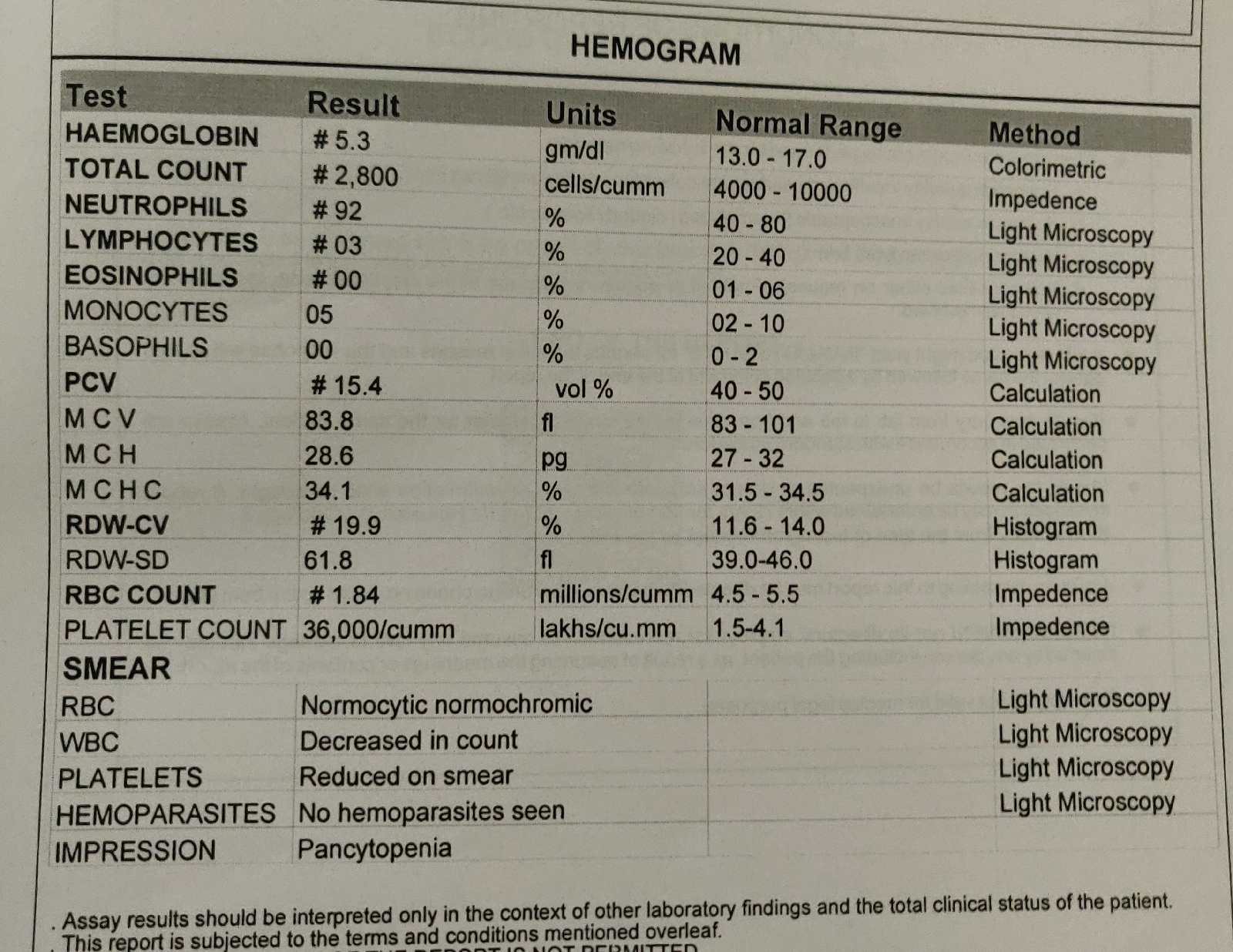
Complete blood picture
Complete urine examination
Chest X-ray
ECG
Ultrasound
Treatment :
Intravenous fluids : Normal saline, Ringer lactate
Injection PANTOPRAZOLE ( proton pump inhibitor)
Injection ZOFER ( Ondansetron - antiemetic)
Injection METROGYL ( Metronidazole )
Injection MONOCEF ( antibiotic)
Tablet DOXYCYCLINE 100 mg/ 3 tablets








Comments
Post a Comment