General Medicine Case Discussion
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings , investigations and come up with a diagnosis and treatment plan.
A 80 year old patient came to the casualty with the chief complaints of :
1. Shortness of breath (grade III) since 3 hours
2. Loose stools - 3 episodes on 19/10/21
3. Fever since 6 days which is associated with chills and rigor.
He used to smoke 18 beedis/day , smoked for 30 years. After he was diagnosed with Tuberculosis (took treatment for 2 years) , he stopped smoking.
He was an alcoholic , took 90ml/day and stopped 1 year back, now takes occasionally during social gatherings.
He had a history of repeated falls 1 year back , for which he went to the government hospital.
Initially the patient was told that he had low blood pressure, then after 5 months , he was diagnosed with hypertension and started taking medications.
He had a history of pedal edema and shortness of breath 1 year back for which he came to KIMS . He was diagnosed with Renal Failure and was on conservative treatment for 4 months, then he stopped taking medication and is only on Tab NODOSIS till now.
Patient had the history of fall 1 week back , no history of loss of consciousness, had a small abrasion on the head.
Patient is complaining of low grade fever since 2 days , intermittent, relieved on taking medication, not associated with chills and rigor.
Patient had constipation for 2 days , took DULCOLAX tablets, had loose stools (3 episodes)
Patient is complaining of Shortness of breath (grade III) and became irritable.
The patient is a known case of Hypertension, is on Tab AMLODIPINE 5mg.
Vitals on admission:
Temperature - 98.4 F
Pulse rate - 92bpm
Respiratory rate- 22/min
Blood pressure- 150/70mm Hg
SpO2 at room air- 90%
GRBS - 120mg/dl
CVS - S1 S2 present, no murmurs
RS -
P/A -
Shape of Abdomen - scaphoid
No tenderness
No palpable mass
CNS - NAD
INVESTIGATIONS :
Rapid Antigen Test for Covid - negative
ABG at 3 AM on 19/10/21:
pH - 7.44
pCO2 - 38.2
HCO3 - 25
pO2 - 57.2
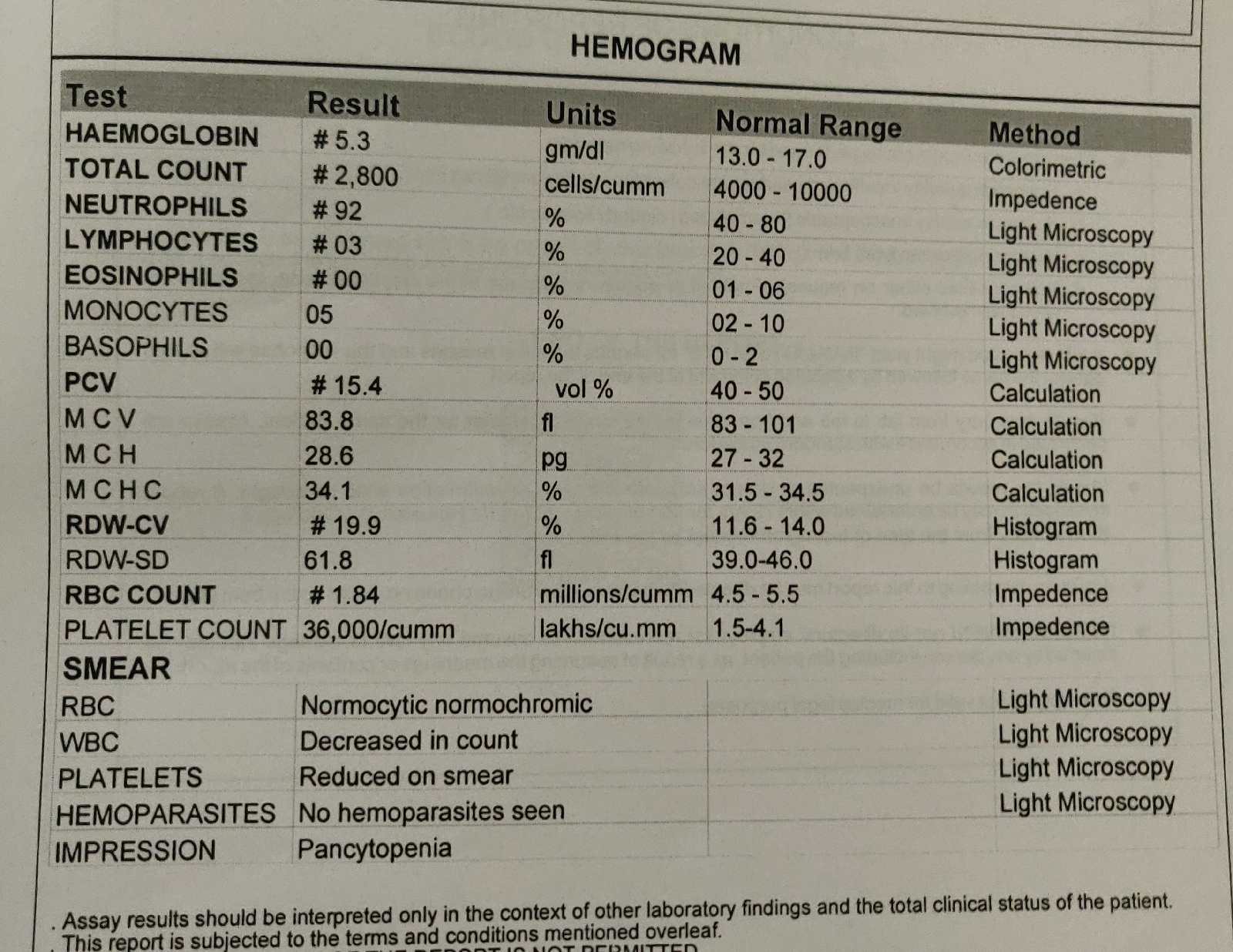
Hemogram:
Hb- 12.7 g/dl
TLC - 22,400
N/L/E - 63/32/02
PLC - 2.45 lakhs
RFT :
Urea - 39
Creatinine- 1.2
Na - 132
K - 3.9
Cl- 92
LFT :
TB - 1.3
DB - 0.5
AST - 28
ALT - 12
ALP - 136
TP - 6
A/G - 0.7
RBS - 118mg/dl
PROVISIONAL DIAGNOSIS :
Community Acquired Pneumonia with K/C/O CKD since 2 years.
History of Pulmonary Koch's 30 years back
K/C/O Hypertension since 2 years
Treatment given :
1. Inj AUGMENTIN 1.2gm/IV/BD
2. Tab AZITHROMYCIN 500mg PO/BD
3. Head end elevation upto 30 degrees
4. O2 supplementation if SpO2 <90%
5. Fluid restriction <1litre/day
6. Salt restriction <2.4g/day
7. Tab AMLODIPINE 5mg PO/OD
8. Tab NODOSIS 500mg PO/OD
9. Nebulization with DUOLIN - 6th hourly
BUDECORT - 8th hourly
10. Tab DOLO 650mg /PO/SOS
11. Monitoring of vitals- 4th hourly
On 20/10/2021 :
Day 2
75 yr/ M
Soap notes
S:
No fever spikes
SOB decreased
Cough decreased
Passed black tarry stools in the morning
H/o DULCOLAX suppository 2 days back
O:
Pt is c/c/c
Temp-96.7 F
BP-160/90mmhg
PR- 97 bpm , regular, normal volume
RR- 27 cpm
SpO2 - 90% at room air
GRBS - 90mg/dl
I/O - 2850ml/1350ml
CVS- S1 S2 +. No murmur
RS- NVBS+, Inspiratory crepts in all areas and wheeze present in bilateral ISA, MSA
P/A- soft, non tender
CNS- NAD
A:
Community Acquired Pneumonia with K/C/O CKD since 2 years
H/o Pulmonary Koch's 30 years back with K/C/O Hypertension since 2 years.
P:
1. Inj AUGMENTIN 1.2 gm/ IV/BD
2. Tab AZITHROMYCIN 500mg/PO/BD
3. Head end elevation
4. O2 supplementation if SpO2 <90%
5. Fluid restriction < 1litre/day
6. Salt restriction <2.4g/day
7. Tab AMLODIPINE 5mg/PO/OD
8. Tab NODOSIS 500mg/PO/OD
9. Nebulization with DUOLIN -6th hourly
BUDECORT - 8th hourly
10. Intermittent CPAP 2nd hourly
11. Tab DOLO 650mg/PO/SOS
12. Vitals monitoring 4th hourly.
On 21/10/2021 :
75 yr/ M
S:
No fever spikes
SOB decreased
Cough decreased
O:
Pt is c/c/c
Temp-96.7 F
BP-120/70mmhg
PR- 74 bpm , regular, normal volume
RR- 27 cpm
SpO2 - 99% on 8 litres of oxygen
GRBS - 84mg/dl
I/O - 900ml/700ml
CVS- S1 S2 +. No murmur
RS- NVBS+, Inspiratory crepts in all areas and wheeze present in bilateral ISA, MSA
P/A- soft, non tender
CNS- NAD
A:
Community Acquired Pneumonia with K/C/O CKD since 2 years
H/o Pulmonary Koch's 30 years back with K/C/O Hypertension since 2 years.
P:
1. Inj AUGMENTIN 1.2 gm/ IV/BD
2. Tab AZITHROMYCIN 500mg/PO/BD
3. Head end elevation
4. O2 supplementation if SpO2 <90%
5. Fluid restriction < 1litre/day
6. Salt restriction <2.4g/day
7. Tab AMLODIPINE 5mg/PO/OD
8. Tab NODOSIS 500mg/PO/OD
9. Nebulization with DUOLIN -6th hourly
BUDECORT - 8th hourly
10. Intermittent CPAP 2nd hourly
11. Tab DOLO 650mg/PO/SOS
12. Vitals monitoring 4th hourly.
On 22/10/21
AMC, Unit 1
Day 4
75 yr/ M
Soap notes
Case seen by :
Dr.Sai Surya(intern )
Dr.Neha (intern )
Dr.Trishaala(intern )
Dr.Varaprasad(intern )
Dr.Srivalli(intern )
Dr.Harika.K (intern )
Dr.Aashitha PG Y 3
Dr.Nikitha PG Y3
Dr.Usha PG Y 3
Dr.Shashikala PG Y3
Dr.Hareen Sr Resident
Dr.Arjun kumar Ass prof
Dr .Rakesh Biswas HOD
S:
No fever spikes
SOB decreased
Cough decreased
O:
Pt is c/c/c
Temp-97 F
BP-120/80mmhg
PR- 80 bpm , regular, normal volume
RR- 27 cpm
SpO2 - 100% on 8 litres of oxygen
GRBS - 82mg/dl
CVS- S1 S2 +. No murmur
RS- NVBS+
P/A- soft, non tender
CNS- NAD
A:
Community Acquired Pneumonia with K/C/O CKD since 2 years
H/o Pulmonary Koch's 30 years back with K/C/O Hypertension since 2 years.
P:
1. Inj AUGMENTIN 1.2 gm/ IV/BD
2. Tab AZITHROMYCIN 500mg/PO/BD
3. Head end elevation
4. O2 supplementation if SpO2 <90%
5. Fluid restriction < 1litre/day
6. Salt restriction <2.4g/day
7. Tab AMLODIPINE 5mg/PO/OD
8. Tab NODOSIS 500mg/PO/OD
9. Nebulization with DUOLIN -6th hourly
BUDECORT - 8th hourly
10. Intermittent CPAP 2nd hourly
11. Tab DOLO 650mg/PO/SOS
12. Vitals monitoring 4th hourly.











Comments
Post a Comment